FDA approves groundbreaking twice-yearly HIV prevention shot
Unlike daily PrEP pills or injections given every two months, the shot could be more appealing to people who struggle with adherence or wish to avoid the stigma associated with daily medication.
The United States' Food and Drug Administration (FDA) has approved a groundbreaking HIV prevention drug that requires just two doses a year, offering new hope in the fight against the virus that continues to infect millions globally.
The medication, called lenacapavir, is the first of its kind and is being hailed as a potential game-changer in HIV prevention, particularly for people at high risk of infection.
More To Read
- UNAIDS hails Kenya–US health framework as major boost for HIV response
- Kenya's HIV statistics (2024)
- German researchers find highly effective HIV antibody
- Zambia, Eswatini first in Africa to receive twice-yearly HIV prevention injection as Kenya eyes approval
- Aid cuts to force Kenya, other African governments to rethink development in 2026
- Tanzanian woman's immune response yields antibody capable of halting most HIV variants
Developed by Gilead Sciences, lenacapavir works by forming a long-lasting "depot" under the skin after two injections in the abdomen. From there, the drug slowly releases into the body over six months, providing continuous protection against HIV.
Unlike daily PrEP pills or injections given every two months, the shot could be more appealing to people who struggle with adherence or wish to avoid the stigma associated with daily medication.
According to AP News, in trials involving thousands of participants at high risk, including young women in South Africa and Uganda, no new HIV infections were recorded among those who received the shot. On the other hand, a control group using daily PrEP pills recorded new infections.
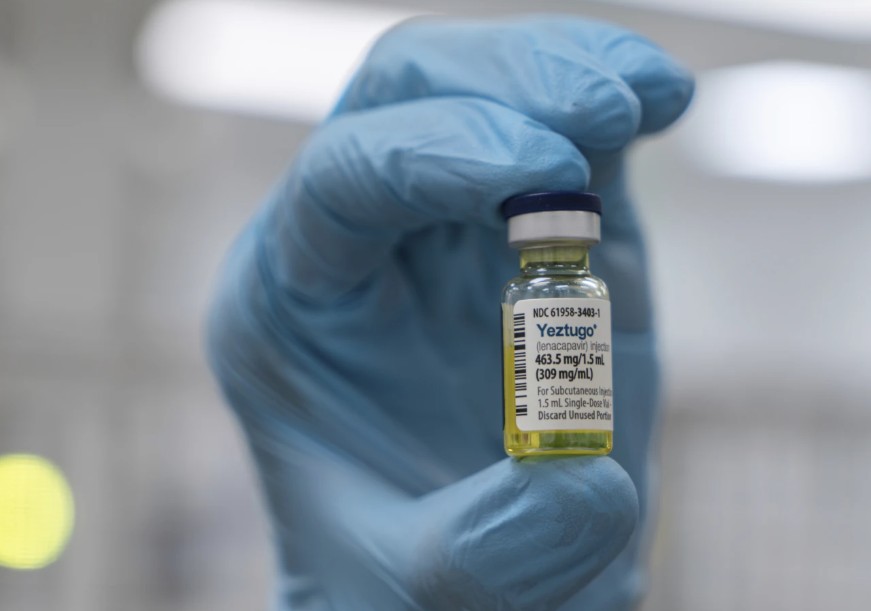
Additional reports indicate that the medication is already used in HIV treatment under the brand name Sunlenca, but its new preventive version will be sold as Yeztugo.
"This really has the possibility of ending HIV transmission," Greg Millett, public policy director at amfAR, The Foundation for AIDS Research, told AP News.
However, before receiving lenacapavir, individuals must test negative for HIV, as the shot is designed to prevent infection, not treat it.
The drug also does not offer protection from other sexually transmitted infections. Mild pain at the injection site is also common, according to experts.
Despite its promise, the rollout of lenacapavir faces serious challenges. Cuts to public health funding in the US, along with reductions in American foreign aid for global HIV programmes, threaten to limit access.
Experts warn that systemic gaps in healthcare infrastructure may make it difficult not only to distribute the drug widely but also to ensure that people return for their next dose every six months.
According to the World Health Organisation (WHO), approximately 39.9 million people were living with HIV globally at the end of 2023.
Similarly, the Joint United Nations Programme on HIV/AIDS (UNAIDS) reported 1.3 million new HIV infections worldwide in 2023.
Top Stories Today














































